Does Lupus Cause Brain Lesions?
 December 29, 2023 | Lupus
December 29, 2023 | Lupus
Does Lupus Cause Brain Lesions?
Lupus, also known as systemic lupus erythematosus (SLE), is an autoimmune disease that can affect various organs in the body. When it affects the brain, it is referred to as neuropsychiatric lupus or neuropsychiatric SLE (NPSLE). NPSLE is a serious manifestation of lupus and can present with a range of symptoms, including headaches, “brain fog,” mood disorders, strokes, seizures, and confusion.
The exact cause of neuropsychiatric lupus is not well understood, but it is believed to involve autoimmune and inflammatory processes. Brain lesions can be observed in lupus patients, particularly in the form of ischemic injury to small-diameter blood vessels in the brain. Prompt diagnosis and treatment of neuropsychiatric lupus are crucial for optimal outcomes. The treatment typically involves immunosuppressive drugs, corticosteroids, and other medications to manage symptoms and control inflammation.
Key Takeaways:
- Lupus, or SLE, is an autoimmune disease that can affect various organs, including the brain.
- When lupus affects the brain, it is called neuropsychiatric lupus or NPSLE.
- NPSLE can cause a range of symptoms, including headaches, mood disorders, strokes, seizures, and confusion.
- Brain lesions can be observed in lupus patients, particularly due to ischemic injury to small blood vessels in the brain.
- Early diagnosis and prompt treatment are crucial for managing NPSLE and improving outcomes.
What is Neuropsychiatric Lupus?
Neuropsychiatric lupus, also known as NPSLE, is a term used to describe the involvement of the central nervous system (CNS) or peripheral nervous system (PNS) in patients with systemic lupus erythematosus (SLE). When lupus affects the brain or spinal cord, it is considered CNS involvement, whereas involvement of the peripheral nerves outside the spinal column is referred to as PNS disease.
NPSLE can present with a wide range of symptoms, from mild non-specific complaints such as headaches and “brain fog” to more severe manifestations like strokes, seizures, and psychosis. It is important to differentiate NPSLE symptoms from those caused by other medical conditions, as lupus-related symptoms can overlap with other common problems. This requires careful evaluation by rheumatologists and other healthcare professionals to determine the underlying cause of the symptoms and provide appropriate treatment.
Common Symptoms of Neuropsychiatric Lupus
Neuropsychiatric lupus (NPSLE) can manifest with various symptoms, indicating its impact on the central nervous system. The most common symptoms associated with NPSLE include:
- Stroke: Resulting from lupus-related inflammation in the blood vessels of the brain, strokes can cause sudden neurological deficits and require immediate medical attention. Patients with NPSLE are more prone to stroke compared to the general population.
- Seizures: Epileptic seizures can occur in individuals with NPSLE, often associated with lupus flares or as a direct result of brain inflammation caused by the disease. Proper management and antiepileptic medications are essential in controlling seizures.
- Sudden Confusion: Cognitive impairment and confusion are frequent symptoms of NPSLE. They can manifest as difficulties with memory, concentration, and problem-solving, impacting daily functioning.
- Psychosis: Some individuals with NPSLE may experience psychosis, which refers to a loss of contact with reality. Symptoms may include hallucinations, delusions, or disorganized thinking and behavior.
- Peripheral Neuropathy: Nerve damage affecting the peripheral nervous system can lead to symptoms such as numbness, tingling, weakness, or pain in the extremities.
In individuals with neuropsychiatric lupus, prompt diagnosis and effective treatment are crucial in managing these symptoms and preventing further complications.
It is important to note that these symptoms can also be present in other medical conditions. Therefore, healthcare professionals must carefully evaluate patients with suspected NPSLE to establish an accurate diagnosis and provide appropriate treatment. Headaches, for instance, can be a symptom of lupus, but they can also stem from migraines, tension headaches, or sinus issues. Similarly, confusion and psychosis can be caused by various factors, including infections or certain medications.
Causes of Neuropsychiatric Lupus
The exact causes of neuropsychiatric lupus (NPSLE) are not fully understood. It is believed to involve a combination of autoantibodies and inflammatory proteins that can reach the brain and cause inflammation. In some cases, lupus-related inflammation can lead to the formation of blood clots, which can affect blood flow to the brain and cause strokes. The activity of lupus, as well as the presence of antiphospholipid antibodies in the blood, can increase the risk of blood clots. Other factors, such as the emotional burden of living with a chronic disease and certain medications used to treat lupus, may also contribute to neuropsychiatric symptoms.
“The exact causes of neuropsychiatric lupus (NPSLE) are still not fully understood, but researchers believe that a combination of autoantibodies and inflammatory proteins play a key role in the development of the condition,” explains Dr. Rachel Johnson, a renowned rheumatologist. “These autoantibodies and inflammatory proteins can cross the blood-brain barrier and trigger inflammation in the brain, leading to the neurological symptoms associated with NPSLE.”
Although the exact mechanisms are not yet fully elucidated, ongoing research continues to shed light on the causes and underlying processes of neuropsychiatric lupus. By further understanding the complexities of this condition, researchers hope to develop more targeted treatments and interventions to improve the lives of individuals living with NPSLE.
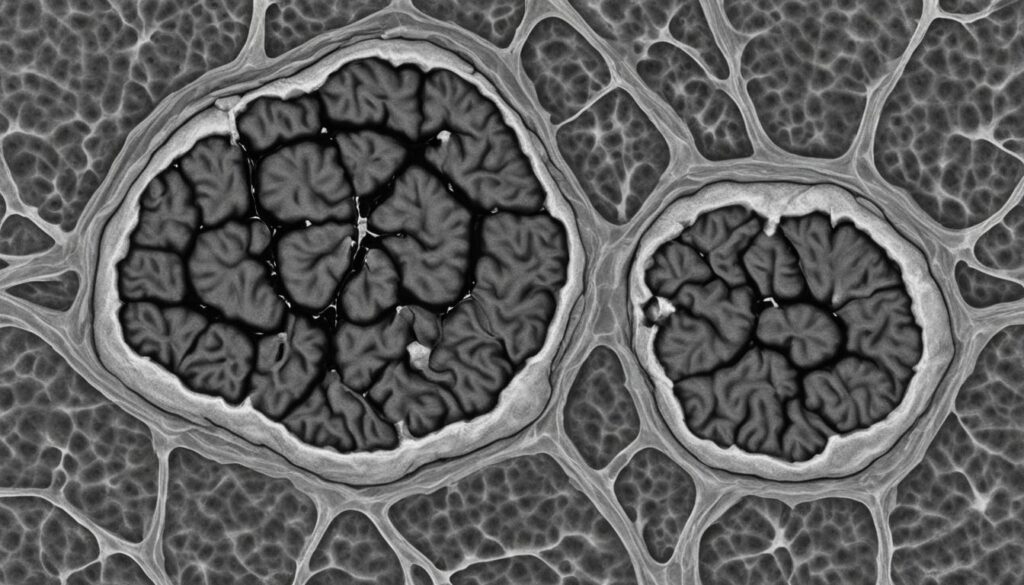
The image above provides a visual representation of the intricate interplay between autoantibodies, inflammatory proteins, and blood clot formation in the context of neuropsychiatric lupus.
Treatment for Neuropsychiatric Lupus
The treatment for neuropsychiatric lupus (NPSLE) depends on the specific symptoms and their underlying cause. When NPSLE is associated with active lupus flares, treatment typically involves the use of glucocorticoids, immunosuppressive drugs, blood thinners, anti-seizure medications, and mood stabilizers.
Glucocorticoids
Glucocorticoids, such as prednisone, are commonly prescribed to control inflammation and manage lupus flares in the central nervous system. These medications help suppress the immune system and reduce inflammation.
Immunosuppressive Drugs
In cases where lupus-related inflammation is severe and persistent, immunosuppressive drugs like cyclophosphamide or mycophenolate mofetil may be used. These medications help suppress the immune system and reduce damage to the central nervous system.
Blood Thinners
In the presence of blood clots, blood thinners may be prescribed to prevent further clot formation. These medications, such as anticoagulants, help improve blood flow and reduce the risk of stroke in individuals with NPSLE.
Anti-Seizure Medications
Seizures, a common symptom of NPSLE, can be managed with anti-seizure medications. These medications help control abnormal electrical activity in the brain and reduce the occurrence of seizures.
Mood Stabilizers
In cases where NPSLE presents with symptoms of psychosis and confusion, mood stabilizers and antipsychotic medications may be prescribed alongside immunosuppressive drugs. These medications help stabilize mood, manage psychosis, and improve cognitive function.
The treatment approach for NPSLE should be individualized, taking into account the specific symptoms, disease activity, and overall health of each patient. Regular monitoring, medication adjustments, and multidisciplinary care involving rheumatologists, neurologists, and other healthcare professionals are crucial for optimal management of neuropsychiatric lupus.
Diagnosis and Treatment Challenges in Neuropsychiatric Lupus
Diagnosing and treating neuropsychiatric lupus (NPSLE) can be a complex task due to the wide range of symptoms associated with this condition and the potential overlap with other medical conditions. NPSLE is diagnosed based on a comprehensive evaluation that includes symptom presentation, physical examination, and laboratory tests. However, doctors need to rule out other possible causes for the symptoms before attributing them to lupus, such as infections or drug-related adverse effects.
The diagnostic process typically involves a thorough assessment, including complete blood counts, antibody testing, imaging studies like magnetic resonance imaging (MRI), and sometimes spinal taps or nerve conduction studies. These tests help doctors evaluate the extent of central nervous system involvement and differentiate NPSLE from similar conditions.
“The diagnosis of NPSLE can be challenging due to the varied symptomatology and potential overlap with other medical conditions.”
Treatment decisions for NPSLE depend on the specific symptoms and their underlying cause. Prompt treatment is crucial to effectively manage NPSLE and prevent complications. Treatment approaches may involve a combination of immunosuppressive drugs, corticosteroids to control inflammation, and other medications to manage specific symptoms like mood disorders or seizures.
However, it is important to note that the treatment decisions for NPSLE should be tailored to each individual’s unique circumstances and may require adjustments over time based on their response to therapy.
Case Study: Diagnostic Challenges in Neuropsychiatric Lupus
A fascinating case study showcases the diagnostic challenges encountered in a male adolescent with a known history of idiopathic thrombocytopenic purpura (ITP) who experienced a seizure and presented with a space-occupying lesion in the brain. The diagnostic process was complicated by multiple potential causes, including abscess formation or an inflammatory process of undetermined etiology.
Imaging studies, such as CT and brain MRI scans, were conducted on the patient to aid in the diagnosis. The MRI image findings revealed specific characteristics, such as a hyperdense lesion with surrounding edema and contrast uptake. Additionally, MR spectroscopy was performed to further evaluate the nature of the lesion.
Despite the diagnostic dilemma, the patient’s medical history, laboratory findings, and imaging results ultimately led to a diagnosis of neuropsychiatric lupus. This complex case highlights the importance of a multidisciplinary approach and comprehensive evaluation when dealing with the diagnostic challenges of neuropsychiatric lupus.
Key MRI Findings:
| MRI Findings | Interpretation |
|---|---|
| Hyperdense lesion | Suggestive of an active inflammatory process |
| Surrounding edema | Indicates tissue swelling and potential disruption of normal neural pathways |
| Contrast uptake | Highlights areas of increased vascularity and inflammation |
The accurate diagnosis of neuropsychiatric lupus in this case further emphasizes the need for a thorough evaluation, including imaging studies, to support clinical findings and improve diagnostic accuracy. Multidisciplinary collaboration among rheumatologists, neurologists, radiologists, and other specialists is crucial in navigating the complexities of neuropsychiatric lupus and ensuring appropriate treatment.
This intriguing case study underscores the importance of meticulous evaluation and the challenges faced when diagnosing neuropsychiatric lupus. Medical professionals must navigate through various possibilities to arrive at a definitive diagnosis. With advancements in medical imaging techniques and a multidisciplinary approach, accurate diagnoses can be made, ultimately leading to targeted treatment and improved patient outcomes.
Conclusion
Neuropsychiatric lupus (NPSLE), a manifestation of systemic lupus erythematosus (SLE), can present with various symptoms and complications, including brain lesions. Diagnosing NPSLE can be challenging due to the complexity of symptoms and the need to differentiate them from other medical conditions. However, prompt diagnosis and treatment are crucial in effectively managing NPSLE and improving patient outcomes.
Treatment for NPSLE often involves a multidisciplinary approach, including the use of immunosuppressive drugs, corticosteroids, and symptom management strategies. These treatment options help control inflammation and reduce the severity of symptoms. Ongoing research and advancements in treatment continue to enhance the prognosis and quality of life for individuals living with neuropsychiatric lupus and its associated brain lesions.
In addition to medical treatment, support from healthcare providers, support groups, and online communities can be invaluable for individuals with NPSLE and their loved ones. These resources provide emotional support, practical advice, and a sense of belonging. Connecting with others who are going through similar experiences can make a significant difference in coping with the challenges of living with NPSLE.
As research progresses, further understanding of NPSLE and its underlying mechanisms will continue to advance. By promoting awareness, facilitating accurate diagnosis, and providing comprehensive treatment and support, we can improve the lives of those affected by neuropsychiatric lupus and its impact on the brain.
FAQ
Does Lupus Cause Brain Lesions?
Yes, lupus can cause brain lesions, particularly in the form of ischemic injury to small-diameter blood vessels in the brain. These lesions can be observed on brain magnetic resonance imaging (MRI) scans.
What is Neuropsychiatric Lupus?
Neuropsychiatric lupus, also known as NPSLE, refers to the involvement of the central nervous system (CNS) or peripheral nervous system (PNS) in patients with systemic lupus erythematosus (SLE). CNS involvement occurs when lupus affects the brain or spinal cord, while PNS disease refers to the involvement of the peripheral nerves outside the spinal column.
What are the Common Symptoms of Neuropsychiatric Lupus?
The common symptoms of neuropsychiatric lupus include stroke, seizures, sudden confusion, psychosis, and peripheral neuropathy. These symptoms can occur during lupus flares in other organs and may require careful evaluation to differentiate from symptoms caused by other medical conditions.
What are the Causes of Neuropsychiatric Lupus?
The exact causes of neuropsychiatric lupus are not fully understood, but it is believed to involve a combination of autoantibodies and inflammatory proteins that can reach the brain and cause inflammation. Lupus-related inflammation can also lead to the formation of blood clots, which can affect blood flow to the brain and cause strokes.
How is Neuropsychiatric Lupus Treated?
Treatment for neuropsychiatric lupus depends on the specific symptoms and their underlying cause. It typically involves the use of glucocorticoids, immunosuppressive drugs, and other medications to control inflammation and manage symptoms. Blood thinners may be prescribed if blood clots are present, while anti-seizure medications and mood stabilizers may be used to manage seizures, confusion, and psychosis.
What are the Challenges in Diagnosing and Treating Neuropsychiatric Lupus?
Diagnosing and treating neuropsychiatric lupus can be challenging due to the wide range of symptoms and the overlap with other medical conditions. It requires comprehensive evaluation, including blood tests, imaging studies like MRI, and sometimes spinal tap or nerve conduction studies. Treatment decisions depend on the specific symptoms and their underlying cause.
What Should Individuals Know about Neuropsychiatric Lupus and its Brain Lesions?
Neuropsychiatric lupus can cause a range of symptoms and complications, including brain lesions. Prompt diagnosis and treatment are essential to manage the condition effectively and improve outcomes. The diagnostic process can be complex and requires careful evaluation. Treatment involves a multidisciplinary approach, often including immunosuppressive drugs and symptom management strategies. Support from healthcare providers and support groups can also be valuable for individuals with neuropsychiatric lupus.
Source Links
- https://www.hss.edu/conditions_neuropsychiatric-sle-lupus-and-brain.asp
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6603070/
- https://www.verywellhealth.com/lupus-and-ms-whats-the-difference-2249979
ABOUT

Hey there! I'm Angela,
I am a survivor of cancer, lupus, fibromyalgia, and a teenage daughter. Join me as I document my experiences and educate the world on my chronic illness journey.