Does Lupus Affect The Liver?
 December 27, 2023 | Lupus
December 27, 2023 | Lupus
For individuals grappling with systemic lupus erythematosus (SLE), the complexities of managing this autoimmune disease extend beyond its more commonly discussed symptoms. Beyond the skin rashes and joint pain often associated with lupus, patients and healthcare providers must pay close attention to organ systems that can silently bear the brunt of autoimmune turmoil. Among these, liver function merits specific scrutiny, as lupus can exert subtle yet significant influence over this vital organ. As we delve into the liver’s vulnerabilities within the context of SLE, a clear understanding of liver involvement becomes crucial for those seeking to navigate the intricacies of this multifaceted disease.
While not universally prominent among symptoms, liver disease related to lupus can reveal itself through a myriad of changes. Liver involvement in lupus patients can manifest through abnormal liver enzymes, reflecting disturbances in this organ’s operation. These disruptions may stem from an array of sources, ranging from medication-induced toxicity to viral infections or concurrent hepatic conditions that can amplify complications. Considering the liver’s pivotal role in detoxifying the body and regulating a cascade of biological functions, recognizing and properly addressing possible liver afflictions is imperative for maintaining overall health in lupus patients.
Key Takeaways
- Liver abnormalities can be a facet of the systemic impact of lupus erythematosus.
- Liver enzyme tests are a fundamental diagnostic tool for assessing liver function in lupus patients.
- Drug toxicity, viral hepatitis, and coexisting hepatic conditions must be considered in the context of lupus and liver health.
- Monitoring of potential liver involvement is essential for comprehensive lupus management.
- Raising awareness of lupus’s potential liver impact empowers patients to seek timely medical evaluation and care.
Exploring the Connection Between Systemic Lupus Erythematosus and Liver Health
Systemic lupus erythematosus (SLE) manifests in varied and often unpredictable ways, branching beyond its more commonly known effects to potentially jeopardize liver health. The interaction between SLE and the liver, though not at the forefront of autoimmune concerns, necessitates a deeper understanding due to its critical implications on overall health management. In this section, we will delve into the sophisticated relationship between SLE and the liver, shedding light on how this autoimmune disease can influence liver function and health.
Understanding Systemic Lupus Erythematosus (SLE)
An individual struggling with SLE faces a relentless assault by their own immune system, which mistakenly targets healthy tissues within the body. This chronic condition, emblematic of the autoimmune disease category, can lead to a kaleidoscope of symptoms and complications due to its systemic nature. It is essential to recognize that the liver, the body’s chemical processing plant, is not immune to the effects of lupus and can exhibit various degrees of liver dysfunction as part of the broader multisystem involvement.
The Liver’s Role in the Body
Known for its remarkable regenerative capacities and vital role in detoxification, the liver is pivotal for maintaining overall physiological balance. It filters toxins, synthesizes blood clotting factors, and helps manage energy by storing and releasing glucose. Within this context, any compromise in liver function or onset of liver abnormalities significantly undermines the body’s ability to perform these essential tasks, making liver health integral to systemic equilibrium and well-being.
How Autoimmune Diseases Can Impact Liver Function
In the labyrinth of liver-related issues, autoimmune diseases carve a challenging path, manifesting as inflammation, and in some cases, as autoimmune hepatitis. The liver cells may be targeted, interrupted, and inflamed, leading to conditions thatspecifically affect the liver, such as lupus hepatitis. These conditions create a complex clinical picture that not only demands specific treatment strategies but also an unerring focus on meticulously managing the delicate balance of liver health within the scope of systemic lupus erythematosus care.
Key Considerations for Liver Health in SLE Patients:
- Monitoring for signs of liver inflammation or damage early in disease progression
- Integrating liver function tests into routine SLE management protocols
- Considering the potential impact of SLE medications on liver health
- Assessing for coexistent autoimmune liver diseases to inform comprehensive care approaches
Addressing the intersection of autoimmunity with liver health is crucial for the holistic treatment of those living with systemic lupus erythematosus. Thoughtful, informed healthcare strategies open the door to better management practices, ensuring that patients grappling with both SLE and its effects on the liver receive the care they deserve.
Identifying Liver Abnormalities in Lupus Patients
For individuals with systemic lupus erythematosus, monitoring liver function is a critical aspect of managing their overall health. Recognizing liver abnormalities in systemic lupus erythematosus is essential, as it may impact the course of treatment and prognosis. A proactive approach towards identifying and understanding these abnormalities can significantly influence patient care.
The Prevalence of Liver Abnormalities in SLE Cases
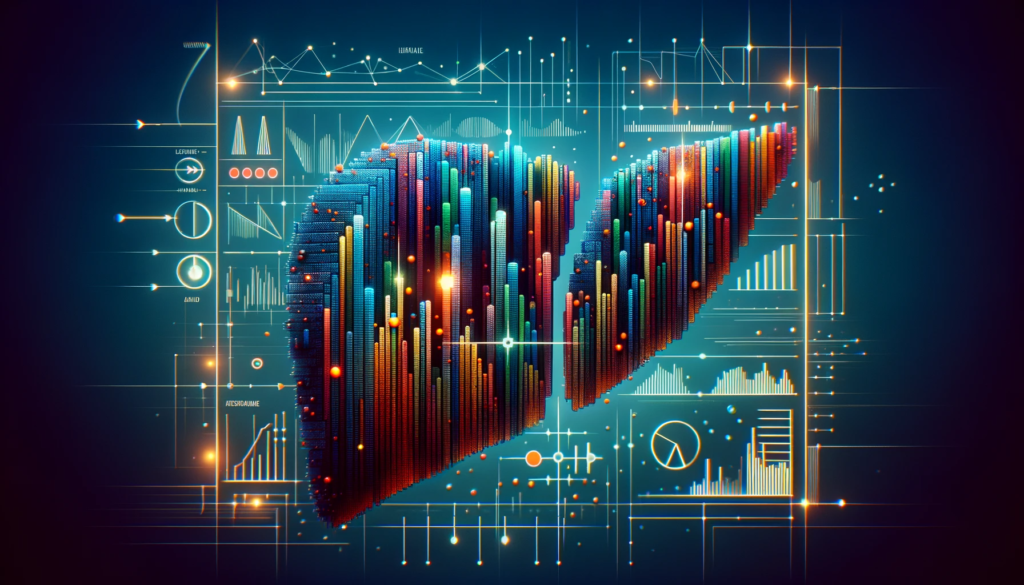
In the realm of systemic lupus erythematosus, the prevalence of liver abnormalities cannot be understated. Often, these abnormalities manifest as variances in blood chemistry, indicating the need for deeper investigation. Liver function tests are frequently used to detect subtle or overt shifts that suggest liver dysfunction in patients with lupus.
Key Indicators of Liver Health: Why Enzyme Levels Matter
Liver enzymes like aspartate aminotransferase (AST) and alanine aminotransferase (ALT) serve as key indicators of liver health. Elevated levels of these enzymes could be indicative of liver inflammation or damage. This elevation is often referred to as elevated liver enzymes, and its persistent presence may pose significant implications for those suffering from lupus.
The Importance of Regular Liver Function Tests for Lupus Patients
Regular monitoring through liver function tests is a crucial component for lupus patients, as it allows for the early detection of liver issues and the timely management of conditions such as lupus hepatitis. These tests are vital in identifying possible liver-related complications and formulating an informed approach to treatment and patient care, thereby mitigating the risk of serious liver dysfunction.
Does Lupus Affect The Liver?
In our ongoing exploration of systemic lupus erythematosus (SLE) and its multifaceted impact on the body, we now turn our attention to a crucial question: does lupus indeed affect liver health? Having established SLE as an autoimmune disease that can potentially impact any organ system, it is imperative to understand how it specifically relates to the liver, a vital organ in the human body. This relationship underscores the complex interplay between autoimmune activity and liver function.
The liver, a powerhouse of detoxification and metabolism, is susceptible to the overarching effects of autoimmune conditions. Within this spectrum, individuals living with lupus may experience an altered liver profile, sometimes resulting in conditions broadly referred to as lupus hepatitis. It is important to discern the nuances between lupus-related liver involvement and other forms of liver disease to ensure accurate diagnosis and treatment.
Autoimmune diseases, including SLE, are known to invoke systemic inflammation, a response that might not exclude liver tissue. Consequently, lupus patients often undergo routine liver function tests (LFTs) to monitor any signs of liver injury or dysfunction. Symptoms of liver involvement, though not exclusive, can sometimes mirror lupus activity in other regions of the body.
Furthermore, lupus treatments, often comprising a range of medications like corticosteroids or immunosuppressants, may bear implications for liver health. Therefore, ongoing vigilance is fundamental for detecting early identifiers of liver dysfunction, which in the case of SLE patients could stem from both the disease itself and its treatment regimen.
Evaluating Liver Disease in SLE Patients: Patients with SLE necessitate careful evaluation which may include—but not limited to—blood tests for enzyme levels, imaging diagnostics, and possibly liver biopsies. These assessments not only serve as hallmarks for detecting liver abnormalities but also guide clinicians in the management of SLE with liver involvement.
Dedicated research continues to grapple with questions surrounding SLE and liver function, striving to provide those affected with clear insights and improved treatment pathways. It becomes clear that lupus can indeed have an attributable effect on the liver, prompting the medical community to uphold a proactive stance in the monitoring and care of lupus patients with respect to liver health.
Common Liver Conditions Associated with Lupus
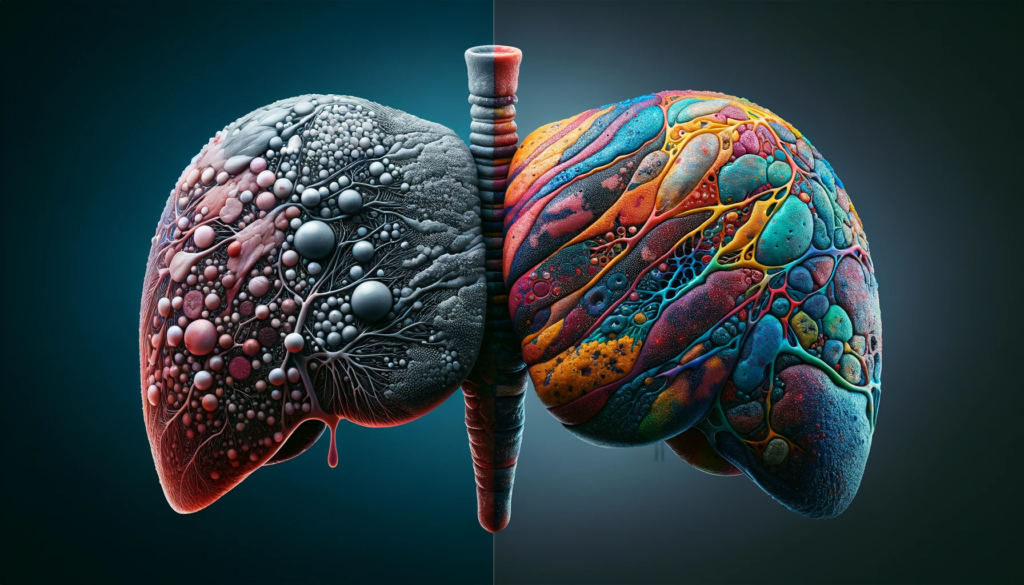
When considering the impact of lupus on the liver, it’s essential to recognize that lupus can affect the liver in several ways, leading to conditions such as lupus hepatitis, autoimmune hepatitis, and fatty liver. Understanding these conditions is critical, not only for correct diagnosis but also for the effective management of liver damage in lupus patients.
Lupus Hepatitis Versus Other Forms of Hepatitis
Lupus hepatitis is unique in that it involves liver inflammation that does not correspond with the overall disease activity of lupus. This form of hepatitis is autoimmune in nature and should not be confused with viral-induced forms. Differentiating lupus hepatitis from hepatitis B or C is a crucial step in ensuring accurate treatment and management.
Understanding Autoimmune Hepatitis in the Context of Lupus
Autoimmune hepatitis, which presents with an immune system attack on liver cells, can coexist with systemic lupus erythematosus (SLE). Clinicians face the challenge of discerning the specific autoimmune process at play—whether it’s primarily due to lupus and the liver’s involvement or a distinct autoimmune hepatitis entity.
When Lupus Leads to Fatty Liver Disease
Fatty liver disease, although commonly associated with metabolic syndromes, can also develop in patients with lupus. It isn’t always a direct result of lupus activity but can be a byproduct of medications, lifestyle, and other health factors in lupus sufferers. Monitoring for fatty liver is an important aspect of managing liver damage in lupus.
| Condition | Features | Association with Lupus | Treatment Considerations |
|---|---|---|---|
| Lupus Hepatitis | Autoimmune inflammation of the liver | Directly related to lupus | Immunosuppressive therapy |
| Autoimmune Hepatitis | Immune system attack on liver cells | May coexist with SLE | Requires careful differentiation from lupus |
| Fatty Liver Disease | Excess fat accumulation in liver cells | Not always direct lupus activity | Metabolic management and lifestyle intervention |
Investigating the Causes of Liver Enzyme Elevation in Lupus
The intricate relationship between lupus and the liver can manifest in elevated liver enzymes, a potential marker of liver dysfunction. While determining the causes of liver dysfunction in lupus patients, medical practitioners must carefully evaluate all contributory factors, including medication effects, drug-induced liver injury, and lifestyle aspects such as alcohol consumption and non-steroidal anti-inflammatory drugs (NSAIDs) usage.
Medication Effects: Drug-Induced Liver Damage in Lupus Treatment
Among the medications used for treating lupus, certain pharmaceuticals stand out for their propensity to induce liver injury. Patients undergoing antitubercular therapy, for instance, require monitoring for signs of drug-induced hepatitis. It is imperative to distinguish drug-induced liver injury from liver issues caused directly by lupus, as this can significantly influence treatment strategies and patient management.
The Impact of Alcohol and NSAIDs on the Liver of Lupus Patients
The consumption of alcohol can pose additional risks for lupus patients. It is known to exacerbate liver inflammation, escalating the challenges in managing lupus-related liver complications. Moreover, the use of non-steroidal anti-inflammatory drugs is a common pain management practice among those with lupus, yet NSAIDs may also impair liver health. Therefore, a comprehensive evaluation is vital to discern the implications of these substances on the liver functions of individuals with lupus.
| Substance | Potential Effect on Liver | Considerations for Lupus Patients |
|---|---|---|
| Antitubercular agents | Induction of hepatitis | Close monitoring for liver enzyme changes |
| Alcohol | Aggravated liver inflammation | Limited intake advised; regular screening for liver damage |
| NSAIDs | Potential to cause drug-induced liver injury | Alternative pain management strategies may be recommended |
Clinical vigilance is key to ensure the proper diagnosis of liver dysfunction. By excluding alcohol and NSAID influence, and accounting for medication effects in the scope of treatment for lupus, healthcare providers aim to safeguard the liver health of their patients. This holistic approach is indispensable in the proactive management of lupus and its potential impact on the liver.
Lupus and Elevated Liver Enzymes: What Patients Need to Know
When navigating the complexities of systemic lupus erythematosus (SLE), it’s imperative for patients to understand the implications of elevated liver enzymes, which can be indicative of several underlying conditions. Increased levels of these enzymes may signal liver dysfunction attributable to lupus hepatitis, other autoimmune liver diseases, or as side effects of lupus medications. Patients, alongside healthcare providers, need to be vigilant in interpreting liver function tests and cognizant of the various factors leading to enzyme alterations.
Interpreting Elevated Liver Enzymes: When Should You Be Concerned?
Elevated liver enzymes are a source of concerns for lupus patients, hinting at potential liver damage or disease. Medical practitioners typically consider enzyme levels that are twice the upper limit of normal as a threshold warranting further evaluation. This additional assessment helps in ruling out the possibility of drug-induced liver injury and in identifying conditions like primary biliary cirrhosis or autoimmune hepatitis.
The Role of Lupus Medications in Liver Enzyme Changes
The relationship between lupus medications and liver enzyme changes is undeniable. Certain drugs used to manage lupus symptoms could negatively impact liver enzymes, emphasizing the need for regular monitoring. Adjustments to treatment plans may be necessary upon detecting abnormal enzyme activity to mitigate negative effects on liver health and overall patient well-being.
Lupus Hepatitis: A Closer Look at Symptoms and Treatments
When it comes to autoimmune conditions affecting the liver, lupus hepatitis is particularly challenging due to its subtle onset and symptomatology. Identifying and addressing lupus hepatitis symptoms, diagnosing liver abnormalities, and defining the right treatment for lupus hepatitis are integral to maintaining liver health and establishing effective management strategies.
Diagnosing Lupus Hepatitis: Understanding the Criteria
Being thorough in diagnosing lupus hepatitis is crucial, as it encompasses an array of liver symptoms that often mimic other conditions. Transaminitis, characterized by elevated liver enzyme levels, typically signals the presence of lupus hepatitis, though it is not exclusively linked to lupus disease activity. Clinicians must engage a comprehensive evaluation process that reviews the patient’s clinical history in full, carefully excluding other potential causes such as drug toxicity and viral infections to accurately diagnose liver abnormalities associated with lupus.
Treating Lupus Hepatitis: Managing Symptoms and Promoting Liver Health
The cornerstone of treatment for lupus hepatitis lies in managing its symptoms effectively and focusing on enhancing liver health long-term. Immunosuppressive therapy may be employed to modulate the autoimmune activity and facilitate symptom management. It is essential to monitor liver function proactively, adjusting treatment strategies in response to follow-up findings. Overall, the prognosis can be favorable, as several cases have reported complete resolution of transaminitis, emphasizing the effectiveness of tailored management strategies in lupus hepatitis care.
Differentiating Between Lupus-Induced and Drug-Induced Liver Damage
The complexity of diagnosing liver disease in systemic lupus erythematosus (SLE) stems from the fact that manifestations can closely resemble those of drug-induced liver injury. It’s imperative for healthcare providers to employ strategic approaches to avoid misdiagnosis and to understand the nuances between drug-induced vs lupus-induced liver damage. This differentiation is critical in prescribing the correct course of treatment and ensuring patient safety.
Avoiding Misdiagnosis: Important Considerations for Physicians
For healthcare professionals, physician considerations play a pivotal role when assessing anomalies in liver function tests (LFTs). Acknowledging the broad clinical presentation of lupus-related liver conditions is necessary to circumvent a false diagnosis of drug-related hepatotoxicity. A thorough patient history including the timeline of symptoms in relation to medication initiation, as well as comprehensive evaluation of all potential causes of elevated liver enzymes, are essential steps in the diagnostic process.
Strategies to Differentiate Between Lupus and Drug Effects on the Liver
To accurately pinpoint the cause behind liver abnormalities, physicians must employ a multifaceted approach. Differentiation strategies include:
- A meticulous review of patient’s medication history and potential hepatotoxic agents
- Careful monitoring of symptom progression with ongoing treatments
- Serial LFTs to track changes and trends that correlate with drug intake or disease activity
- Autoimmune serologies to identify possible overlap syndromes requiring distinct interventions
Implementing these measures is vital for confirming a specific diagnosis and tailoring treatment plans appropriately. Here’s an illustration of how a healthcare provider can categorize liver anomalies:
| Clinical Feature | Lupus-Induced Liver Damage | Drug-Induced Liver Damage |
|---|---|---|
| Onset of symptoms | Gradual, with lupus flare | Rapid post-medication |
| Liver Enzyme Patterns | Autoimmune markers present | Often isolated enzyme elevation |
| Response to treatment | Improves with SLE management | Eases upon drug cessation |
| Imaging and Histology | May show chronicity | Often acute changes |
| Concomitant symptoms | Other organ involvement | Usually liver-specific |
By closely evaluating these aspects, healthcare professionals can provide a more accurate diagnosis of liver involvement in SLE and customize a suitable management plan for their patients.
The Long-Term Outlook for Lupus Patients with Liver Involvement
The long-term health outcomes for lupus patients with liver involvement are subject to various factors including disease activity, response to treatment, and the presence of overlapping conditions. Systemic lupus erythematosus (SLE) impacts individuals differently, making it essential to monitor liver function closely over time.
Liver involvement in lupus patients is a complex facet of the disease that requires ongoing medical attention and comprehensive care strategies. Understanding the future implications of liver abnormalities can be pivotal for patients and healthcare providers alike. Let us explore the long-term prognosis for those living with both lupus and liver complications.
Survival rates and quality of life for lupus patients with liver involvement can be influenced by a range of variables. Early detection and intervention, lifestyle adjustments, and adherence to treatment protocols are essential components of successful long-term management. The managed care approach for lupus patients prioritizes regular evaluation and treatment modification based on disease progression and liver condition.
| Prognostic Factor | Impact on Long-Term Outlook |
|---|---|
| Disease Activity Control | Effective management of lupus activity correlates with reduced liver complications and improved long-term outcomes. |
| Treatment Response | Patients responsive to lupus therapies tend to exhibit fewer liver-related issues and better overall prognosis. |
| Lifestyle Factors | Lifestyle choices such as diet, exercise, and avoidance of alcohol contribute to healthier liver function and longevity. |
| Co-existing Conditions | Additional liver conditions like fatty liver disease or autoimmune hepatitis can significantly alter the disease course and prognosis. |
| Medical Monitoring | Regular liver function tests and proactive medical intervention can enhance management and long-term outlook. |
It is noteworthy that the psychological impact of chronic liver disease in lupus patients is a critical consideration. Maintaining mental and emotional well-being is integral to achieving a balanced life, despite the challenges of SLE with liver involvement. Counseling and support groups can be valuable resources for patients navigating these conditions.
In summary, while systemic lupus erythematosus combined with liver disease can be challenging, with personalized care and vigilant monitoring, patients can look forward to a more optimistic long-term outlook. Modern advances in medical therapies and a better understanding of the disease dynamics continue to improve the quality of life for those affected.
The Role of Imaging and Biopsies in Diagnosing Lupus-Related Liver Disease
Crucial in the management and assessment of systemic lupus erythematosus (SLE) is the early and accurate determination of potential liver complications. As such, advanced diagnostic tools play a pivotal role in the detection and treatment of lupus-related liver disease. Imaging for lupus-related liver disease, particularly through ultrasonography, has become a cornerstone in identifying early signs of hepatic involvement.
Utilizing Ultrasonography for Liver Assessment in SLE Patients
Ultrasonography stands out as a non-invasive, readily accessible form of imaging that allows for a comprehensive view of liver health. It is favored for its ability to detect aberrations in the liver’s echotexture, the presence of masses, and symptoms indicative of portal hypertension—a common concern in SLE patients. Ultrasonography in SLE not only helps in monitoring the known effects of the disease on the liver but also serves to flag early warnings of liver distress, prompting timely intervention.

The Necessity of Liver Biopsies for Definitive Diagnosis
When abnormalities persist or when the results from non-invasive methods such as ultrasonography are inconclusive, clinicians may turn to liver biopsies. This procedure offers a highly definitive diagnosis by extracting tissue samples directly from the liver, which can then be microscopically examined for specific pathological changes.
| Condition | Ultrasound Features | Importance of Biopsy |
|---|---|---|
| Autoimmune Hepatitis | Homogeneous texture; normal to increased liver size | Essential for diagnosis and grading severity |
| Fatty Liver Disease | Increase in echogenicity; Diffuse brightness | Required to rule out NASH, determine extent |
| Primary Biliary Cirrhosis | Irregular texture; may show nodularity | Confirms diagnosis, aids in staging |
Through liver biopsies, the definitive diagnosis of conditions such as autoimmune hepatitis, primary biliary cirrhosis, and fatty liver disease can be made. Each of these conditions may present alongside lupus, complicating the clinical picture. Thus, liver biopsies act as a decisive tool in not just delineating the cause of hepatic abnormalities, but also in charting an effective treatment path for the patient.
Managing Co-occurring Liver Diseases in Lupus Patients
The intricate interplay between lupus and hepatic health challenges both patients and healthcare providers. The emergence of co-occurring liver diseases alongside lupus catalyzes a multi-disciplinary approach to medicine. With the rise in the incidence of overlap syndromes, a nuanced understanding of diagnostic and therapeutic strategies becomes ever so critical.
Confronting Overlap Syndromes: When Lupus Meets Other Liver Diseases
Overlap syndrome refers to the presence of additional liver conditions such as autoimmune hepatitis or primary biliary cirrhosis alongside systemic lupus erythematosus. Such syndromes demand comprehensive and tailored approaches to managing liver diseases, as therapies for one condition may exacerbate the other. Here, the spheres of rheumatology and hepatology intersect, creating a complex tapestry of care necessities.
The following table delineates common overlap syndromes and their respective characteristics, setting the stage for informed decision-making.
| Lupus-related Liver Disease | Symptoms | Treatment Adjustments |
|---|---|---|
| Autoimmune Hepatitis (AIH) | Fatigue, Jaundice, Abdominal Pain | Immunosuppressive Therapy |
| Primary Biliary Cirrhosis (PBC) | Pruritus, Dry Eyes and Mouth, Hepatomegaly | Ursodeoxycholic Acid Administration |
| Non-alcoholic Fatty Liver Disease (NAFLD) | Usually Asymptomatic, Detected on Liver Function Tests | Lifestyle Modification, Consider Medication Review |
Adapting Lupus Treatments to Accommodate Liver Complications
When navigating liver complications, adaptation of lupus treatments is imperative. Certain medications may need to be modulated to mitigate hepatic strain without undermining lupus management—adapting doses or replacing treatments that invoke hepatotoxicity with those more liver-friendly. Each patient’s liver enzymes, symptoms, and overall health must shape their unique therapeutic path.
Ultimately, the key to managing liver diseases in lupus patients lies in vigilant observation, cross-specialty collaboration, and personalized treatment regimens. Empowerment through education offers the patient a significant role in their care, promoting adherence and optimal outcomes. And as healthcare continues to evolve with advances in understanding and technology, so too will the strategies for managing these complex co-conditions.
Conclusion
Throughout this discussion, the intricate relationship between systemic lupus erythematosus (SLE) and liver health has been scrutinized from multiple perspectives. We recognize that SLE is a complicated autoimmune disease capable of affecting the liver alongside other organs. The potential for liver involvement in lupus patients emphasizes the need for proactive management, including regular monitoring of liver enzymes to detect abnormalities early. Conditions such as lupus hepatitis, autoimmune hepatitis, and fatty liver disease highlight the spectrum of liver abnormalities associated with lupus and underscore the critical role of accurate diagnosis and individualized treatment.
As we explored various aspects of SLE and liver health, the importance of differentiating between lupus-induced and drug-induced liver damage became evident, avoiding misdiagnoses and directing patients towards the most effective treatment strategies. The integration of advanced diagnostic tools like ultrasonography and liver biopsies plays a pivotal role in confirming the presence of liver diseases and adjusting medical management accordingly. Additionally, managing co-occurring liver diseases in lupus patients requires an interdisciplinary approach, ensuring that treatment regimens are adaptable to the evolving needs of each patient.
Ultimately, the journey of living with lupus and its potential impact on liver health is unique to each individual. Patients and healthcare providers must work in tandem to navigate this complex landscape, remaining vigilant and responsive to changes in liver function. By cultivating an understanding of lupus and its possible effects on liver health, patients are better equipped to advocate for their well-being, striving for an improved quality of life.
Frequently Asked Questions
Does Lupus Affect The Liver?
Yes, systemic lupus erythematosus (SLE), an autoimmune disease, can affect liver function and lead to liver involvement, potentially causing various forms of liver disease in lupus patients.
How are Systemic Lupus Erythematosus and Liver Health Connected?
SLE can cause liver abnormalities and dysfunction due to autoimmune attack on liver cells, drug-induced liver injury, or the presence of co-existing liver conditions such as fatty liver, cirrhosis, and autoimmune hepatitis.
What Liver Abnormalities Might Lupus Patients Experience?
Patients with lupus might experience elevated liver enzymes, which indicate inflammation or damage in the liver. Other liver abnormalities associated with SLE include lupus hepatitis, autoimmune hepatitis, and fatty liver disease.
What is the Significance of Liver Enzyme Levels in Lupus Patients?
Elevated liver enzymes, such as AST and ALT, serve as key indicators of liver health in lupus patients. They can signal liver conditions that may require further investigation and management.
Why are Regular Liver Function Tests Important for Lupus Patients?
Regular liver function tests are crucial for monitoring the liver’s condition in lupus patients and for detecting potential issues early to facilitate timely intervention.
How Do Lupus Hepatitis and Other Forms of Hepatitis Differ?
Lupus hepatitis is characterized by liver inflammation specifically associated with lupus and not by viral infections like hepatitis B or C. It must be differentiated from other forms of hepatitis, which have different causes and treatment approaches.
What Role Can Lupus Medications Play in Liver Enzyme Changes?
Some medications used to treat lupus can cause elevated liver enzymes or toxicity, leading to liver injury. Monitoring liver enzymes is important to differentiate between lupus activity and drug-induced liver damage.
How are Elevated Liver Enzymes Interpreted and Managed in Lupus Patients?
Elevated liver enzymes might indicate underlying liver dysfunction, necessitating further evaluation to rule out causes such as drug-induced liver injury, primary biliary cirrhosis, and autoimmune hepatitis. Treatment may involve adjusting or discontinuing certain medications.
What is Involved in Diagnosing and Treating Lupus Hepatitis?
Diagnosing lupus hepatitis involves ruling out other causes for elevated liver enzyme levels and considering the patient’s medical history and liver symptoms. Treatment typically focuses on reducing inflammation and managing liver health.
How Can Physicians Avoid Misdiagnosis Between Lupus-Induced and Drug-Induced Liver Damage?
Physicians must thoroughly review a patient’s clinical history, monitor medication effects, and perform serial liver function tests to distinguish between lupus-induced and drug-induced liver damage.
What is the Role of Imaging and Biopsies in Diagnosing Lupus-Related Liver Disease?
Imaging, especially ultrasonography, helps assess structural liver changes in SLE patients, while liver biopsies might be used for a definitive diagnosis when non-invasive methods are inconclusive.
How are Co-occurring Liver Diseases Managed in Lupus Patients?
Managing co-occurring liver diseases involves integrated care that may require adapting lupus treatments to address both lupus and liver complications while coordinating among healthcare specialists.

Hi there. I’m Angela…and I live daily with chronic illness. For the longest time, I suffered in silence for fear of being judged or criticized. When I finally started opening up, I realized that I’m not alone in all of this and if you have a chronic illness, neither are you!
ABOUT

Hey there! I'm Angela,
I am a survivor of cancer, lupus, fibromyalgia, and a teenage daughter. Join me as I document my experiences and educate the world on my chronic illness journey.